July 25, 2025 — The United States, the world’s wealthiest nation, continues to grapple with a healthcare system that leaves millions struggling to access affordable, quality care. Despite advancements in medical technology and a robust economy, systemic flaws in the U.S. healthcare structure are failing its people, exacerbating inequality, and driving preventable health crises.
Skyrocketing Costs and Unequal Access
The cost of healthcare in the U.S. remains the highest globally, with per capita spending exceeding $12,500 annually, nearly double that of comparable developed nations, according to the OECD. Yet, outcomes lag: life expectancy in the U.S. is 77.5 years, lower than countries like Japan (84.7) or Canada (82.3). For many Americans, the system’s reliance on private insurance tied to employment leaves gaps that prove catastrophic.Approximately 26 million Americans—8% of the population—remained uninsured in 2024, per the Kaiser Family Foundation. Even insured individuals face crushing out-of-pocket costs, with deductibles averaging $1,900 for single coverage plans. Stories of families bankrupted by medical bills or forced to ration medications like insulin, which can cost over $300 per vial without coverage, are all too common.
Structural Inequities and Disparities
The system disproportionately fails marginalized groups. Black Americans, for instance, face maternal mortality rates three times higher than their white counterparts, with 39.8 deaths per 100,000 live births, according to the CDC. Rural communities, where hospital closures have surged—over 140 since 2010—often lack access to basic emergency care, forcing patients to travel hours for treatment.Administrative inefficiencies further strain the system. The U.S. spends 8% of healthcare dollars on administration, compared to 1-3% in peer nations, bloating costs without improving care. Meanwhile, profit-driven insurance companies deny claims at alarming rates, with some studies showing up to 20% of claims rejected for dubious reasons.

The Mental Health Crisis
Mental health care remains a glaring weak spot. With only 28,000 psychiatrists nationwide for a population of 330 million, access to mental health services is severely limited. The National Alliance on Mental Illness reports that 60% of adults with mental health conditions received no treatment in the past year, contributing to rising rates of suicide and substance abuse.
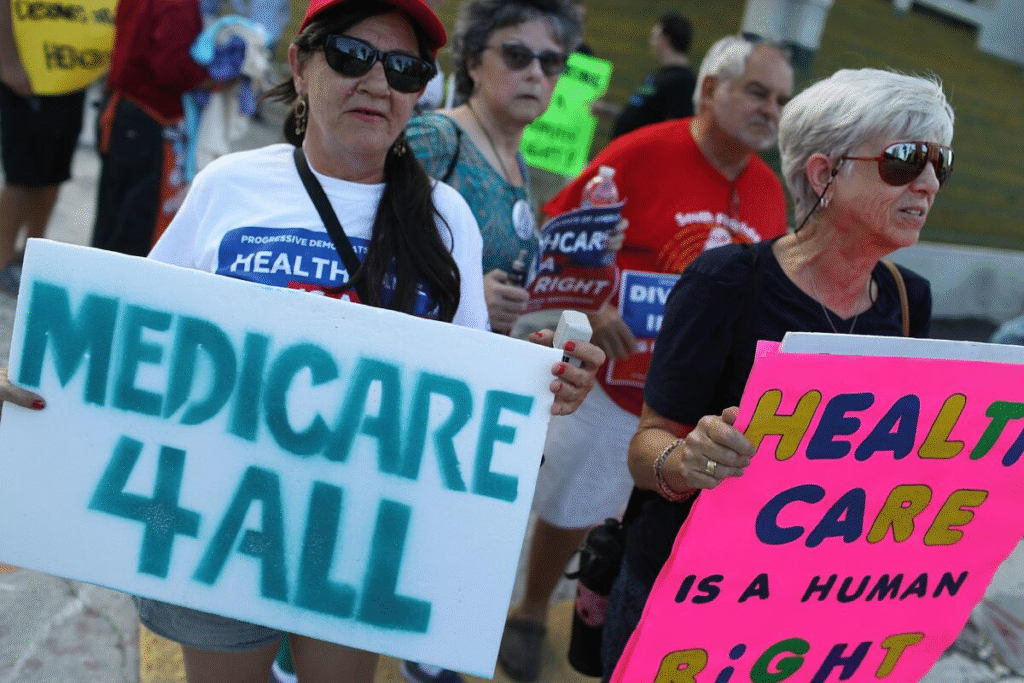
Policy Stagnation and Public Frustration
Efforts to reform the system, such as expanding Medicare or implementing a single-payer model, remain politically divisive. The Affordable Care Act (ACA) reduced the uninsured rate, but its patchwork approach hasn’t addressed root causes like price gouging by hospitals and pharmaceutical companies. Public frustration is evident: a 2024 Gallup poll found 70% of Americans believe the healthcare system is “failing to meet their needs.”
The American healthcare system is a complex and often frustrating beast, and there are plenty of lesser-known aspects that can spark outrage once you dig into them. Here are some things that might make you upset, based on systemic issues, inefficiencies, and inequities that persist:
- Medical Debt is a Leading Cause of Bankruptcy: Despite the Affordable Care Act, medical debt remains a massive issue. About 41% of Americans have some form of healthcare debt, and studies estimate that 60% of bankruptcies in the U.S. are tied to medical bills. Even insured people can face crippling costs due to high deductibles, out-of-network charges, or uncovered treatments. Surprise billing—where patients get hit with unexpected charges from out-of-network providers, even in emergencies—still happens, though recent laws like the No Surprises Act (2022) have tried to curb it.
- Price Gouging is Rampant: The same procedure or medication can cost wildly different amounts depending on where you are or who’s billing. For example, a 2018 study found that the price of an MRI can range from $500 to $2,600 in the same city, with no clear correlation to quality. Drug prices are another sore spot: the U.S. pays more for prescription drugs than any other developed country. Take insulin—its price has skyrocketed over 1000% since 2002, even though the drug’s been around for decades.
- Administrative Waste Eats Up Billions: The U.S. spends about 8% of healthcare dollars on administration—think billing, insurance processing, and red tape—compared to 1-3% in peer countries like Canada or the UK. This translates to roughly $400 billion annually that could be spent on actual care. The complexity of dealing with multiple insurers, each with their own rules, drives up costs for providers and patients alike.
- Racial and Socioeconomic Disparities Persist: Black and Hispanic Americans are more likely to be uninsured (10.6% and 16.7% uninsured rates in 2023, respectively, vs. 7.6% for white Americans). Maternal mortality rates are shockingly high for Black women—49.7 deaths per 100,000 live births compared to 19.1 for white women (2021 data). Rural areas, often poorer, face hospital closures at an alarming rate—over 140 rural hospitals have closed since 2010, leaving communities without access to emergency care.
- Profit Motives Over Patient Care: Many hospitals and insurance companies operate as for-profit entities, which can lead to prioritizing lucrative procedures over preventive care or affordable treatment. Private equity firms have been buying up hospitals and physician practices, often cutting staff or services to boost profits. A 2021 study linked private equity-owned nursing homes to worse patient outcomes, including higher mortality rates.
- Denial of Claims is a Business Model: Insurance companies often deny claims as a first step, banking on patients or providers not appealing. A 2023 report showed that 17% of in-network claims were initially denied by insurers, with many denials overturned only after lengthy appeals. This delays care and burdens patients with stress and paperwork.
- Mental Health Care is Woefully Underfunded: Mental health services are often not covered adequately by insurance, and there’s a severe shortage of providers. Over 60% of adults with mental illness didn’t receive treatment in the past year, per 2022 data, and 25% of those seeking care couldn’t access it due to cost, availability, or coverage issues.
- The Opioid Crisis Was Fueled by Corporate Greed: The healthcare system played a role in the opioid epidemic, with pharmaceutical companies like Purdue Pharma aggressively marketing drugs like OxyContin while downplaying addiction risks. Between 1999 and 2020, over 500,000 Americans died from opioid overdoses, and the system’s slow response left millions struggling with addiction and inadequate treatment options.
A Path Forward?
Experts argue for bold reforms, including price transparency, regulating drug costs, and expanding public options. However, entrenched interests—insurance giants, pharmaceutical companies, and hospital conglomerates—wield significant lobbying power, spending over $700 million annually to influence policy, per OpenSecrets.As the 2026 midterms approach, healthcare remains a top voter concern. For now, millions of Americans continue to navigate a system that too often prioritizes profit over people, leaving them one illness away from financial ruin or worse.


